Vitamin D is known as the sunshine vitamin. It is a steroid hormone that is created from cholesterol when your body is exposed to light. A large percentage of the population is also deficient in vitamin D. It is also not commonly found in many food sources, so reaching the daily recommended intake could require dietary supplementation. Food sources that do have vitamin D include fatty fish – such as mackerel, salmon and cod – as well as fortified milk and fortified cereal. Vitamin D helps your body use calcium and is fundamental in having strong teeth and bones. Low vitamin D can lead to chronic fatigue, heart disease, and poor bone development.
What is Vitamin D?
Vitamin D is not a vitamin it is a secosteroid with a hormone-like activity that is made within the body. It regulates over 200 genes within the body and is necessary for growth, development and immune protection. It is an integral part of immune function, increasing neuromuscular function, improving mood, protecting the brain against toxins and possibly lowering pain. There are two forms of vitamin D2 (ergocalciferol) and D3 (cholecalciferol). Its discovery began with a boom in rickets amongst children during the Industrial Revolution. With a movement from farm life to smoggy city factory life exposure to sunlight decreased drastically.
In 1822 a Polish physician noted that children working in factories in Warsaw and or living in the smog-filled city had drastically increased cases of rickets over children who lived and worked in the countryside, his recommendation was to increase exposure to sunlight. Though it is more prevalent today, vitamin d deficiency has been around for thousands of years, it is hypothesized that Neanderthals exhibited bone deformations that can be attributed to rickets.

Main Functions and Benefits of Vitamin D
Vitamin D Role in Calcium Metabolism
Having active vitamin D in the body increases the absorption of calcium in the gut as well as decreasing its excretion from kidneys. This is how low D3 levels with time will lead to soft bones and poor bone structure. Although it is often recommended to supplement with calcium, it is often not the nutrient that is lacking from the body. It is the lack of vitamin D that is preventing Calcium uptake resulting in deficiencies with both nutrients.
Supports Healthy Bone
Without proper serum levels of calcitriol, bones become soft and more prone to fractures. Pain increases in joints and the development of arthritis greatly increases. Vitamin D helps to keep bones strong by providing the calcium that they need for their development, preventing bone mineral loss as well as reducing oxidative stress and free radical damage which in turn decreases inflammation and diminishes pain. Calciferol helps with the prevention of osteomalacia, osteoporosis as well as aiding in healing fractures and other bone problems.
Supporting Healthy Teeth and Preventing Cavities
Vitamin D puts calcium-phosphorus into teeth, helping to maintain good detention, preventing tooth decay and gum disease. The presence of this essential hormone in the body also blocks a parathyroid hormone which reabsorbs bone tissue resulting in porous and fragile bones.
Immune Boosting
One of the first benefits of vitamin D was its benefit in the prevention of rickets in children. Though very uncommon, as children spend more time inside than outside supplementing with vitamin D and consuming whole foods rich in it, such as cod liver oil and eggs can strengthen the immune system of the child and not only prevent rickets but also aid them in fighting off various infections, it is cancer-fighting and fights off free radicals that are persistent in the system
Vitamin D with vitamin A has been shown to reduce the incidence of colds.
Supports Mental Health
It provides proper nutritional support for the nervous system and has been shown to reduce signs of depression and improve mood. Vitamin D3 has also been very promising in boosting brain plasticity and cognitive performance, especially amongst individuals at-risk of or with dementia.
Some individuals with anxiety develop muscle spasms, vitamin D combined with A is very beneficial at preventing this occurrence.
Vitamin D2 and Vitamin D3
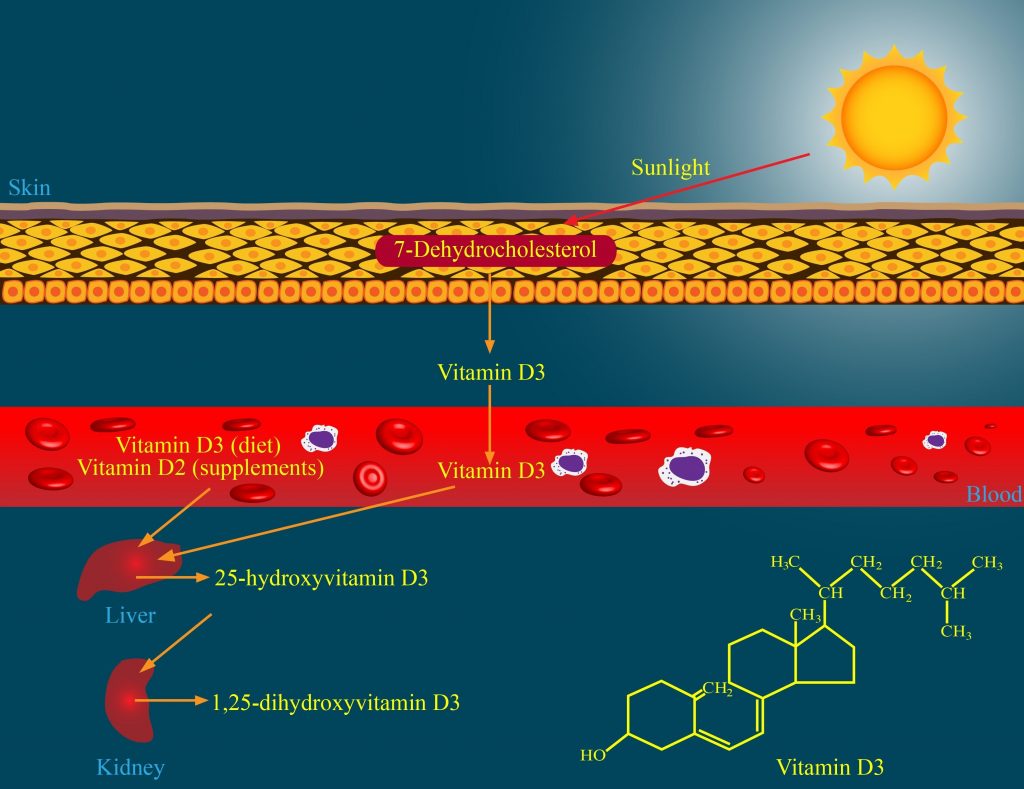
There are two forms of this hormone, vitamin D2 (ergocalciferol) and D3 (cholecalciferol). Both of them are available to us through the consumption of food, however, only D3 is produced by the skin from UVB radiation. Although both forms of Vitamin D supplements turn into calcitriol (the active form of the vitamin in the body), it is when cholecalciferol is supplemented that the concentration of 25(OH)D is profoundly raised and it has a longer half-life then D2. D2 will require more frequent dosages to bring up the elevation to levels that are sufficient to the body.
How Vitamin D gets Absorbed by the Body
Both vitamin D2 and D3 are absorbed though into the intestinal lining after ingestion with the assistance of bile and other fats. From there they first arrive at the liver where they are metabolized into 25-hydroxyvitamin D [25(OH)D] also called calcidiol. Then in the kidneys, it is converted into 1,25 dihydroxyvitamin D [1,25 (OH)2 D] a hormone known as calcitriol. One of the calcitriol’s main functions is regulating calcium in the body. The benefits of vitamin D are then displayed on the body by entering circulation and travels to the main areas of calcium tissue uptake; small intestine and bones. The small intestine has receptors for D3, these activated receptors allow for the absorption of calcium through the intestines.
“More than three-fourths of all Americans are vitamin d-deficient.”
―John Cannell, Athlete’s Edge: Faster, Quicker, Stronger with Vitamin D
If there is not enough calcium in the blood, parathyroid hormone and calcitriol will move to bones and signal the release of calcium from bones as a way to maintain intracellular and extracellular calcium concentrations and supply nerves and muscles with the calcium they need. However, this also leaves the bones thin, brittle and prone to breakage.
When there is sufficient calcium in the diet and body, calcitriol along with parathyroid hormone will be regulated and calcitriol production and activity is low. When calcium is lacking in the body its production is high. When the body is deficient in vitamin D, calcium and phosphorus are also released from the bones to enter the kidney to bring up serum levels. This makes the assessment of serum levels of calcium and phosphorus a flawed way to assess vitamin D status.
How Sunshine turns into a Hormone
Between 50-90% of the vitamin D that is found in the body is obtained from sunlight exposure. Vitamin D3 also known as cholecalciferol, is synthesized by UV radiation of 7-dehydrocholesterol to pre-vitamin D3. High concentrations of melanin affect UVB radiation and reduce the skin’s ability to produce D3 as does aging, sunblock, windows, and clothing.
Regular exposure to sunlight, about 15-20 minutes without the use of sunscreen for 3-4 times a week, with 40% skin exposure when the sun is in your hemisphere. During winter months as well as early spring and late fall supplementing or making sure that your diet is rich in the nutrient is necessary to keep up serum levels (Perez – Lopez, F.R., et al., 2012) (Naeem, Z., 2010).
Calcification
A decrease in Vitamin D and an oversaturation of calcium can often result in calcification to the breast, arterial plaque, as well as other areas in the body as calcium, cannot be properly utilized and metabolized by the body. Moreover, if there is too much Vitamin D in the system due to toxicity, calcification within the body can also occur. Therefore it is essential to be tested once a year for serum Vitamin D levels especially if one is on vitamin d supplements. Calcium ion serum testing should also be conducted once a year to monitor the amounts that are in the body and if there is a possibility of an overdose of vitamin d (too much vitamin D can lead to bone calcification).
Common Reasons for Vitamin D Deficiency
One in eight individuals has a deficiency in this vitamin. The active form of this prohormone is calcitriol or 1,25-dihydroxyvitamin which we measure through serum levels in the body. Insufficient serum levels are anything lower than 20-29 ng/ml. The most at-risk individuals are those who spend most of their time indoors (at work, in transportation, at home, etc), are covered largely by clothing, use sunblock as a manner of usual practice, have darker skin, are overweight, older individuals and those who regularly avoid the sun by using umbrellas, hats, etc. The further you live from the equator the more vitamin D you will need to supplement with, particularly during the fall, winter and spring months. Often the recommended dosages are far to low from what the body requires to function optimally (Naeem, Z., 2010).
Lack of Exposure to the Sun
People who spend a lot of time indoors during the day. For example: If you’re housebound, work nights or are in the hospital for a long time.
People who cover their skin all of the time. For example: If you wear sunscreen or if your skin is covered with clothes.
People that live farther from the Equator. This is because there are fewer hours of overhead sunlight the further you are from the equator.
Age-Related Deficiency
Aging leads to a decline in the body’s ability to convert to create this particular hormone. As one age, the skin becomes ever thinner and over time its ability to produce vitamin D3 from sunlight decreases to almost half of what it was capable of during its youth. With the liver and kidneys also declining in their function the conversion of sunlight to active calcitriol also decreases making it very important to older individuals to supplement. Exposure to sunlight will also increase as 15 minutes may not be enough to produce sufficient D3.
Breast Milk Leading to Deficiency
Breast milk is the best thing that can be given to a newborn baby, however, if the nursing mother is deficient in any nutrient, including vitamin D, the child will not receive sufficient nourishment. If the nursing mother knows she is deficient in vitamin D, she should take a vitamin D supplement and consider supplementing the Infants with a supplement – there are infant vitamin D drops. To make sure that you choose the right supplement and dosage consult your qualified pediatrician or health care, provider. A fortified formula can be an alternative, but if the mother can provide breast milk, a simple vitamin D supplementation would be best.
Obesity and Excess Fat
Excess fat accumulation makes one more susceptible to developing coronary heart disease, hypertension, metabolic syndrome, diabetes, osteoarthritis, and a deficiency in Vitamin D. Individuals who have higher BMI have been shown to have much lower levels of serum level D. Obese individuals have greater stores of active D in adipose tissues (fat) which serves as a repository for the vitamin, therefore more supplementation is required to saturate the body. Most standard guidelines do not take this into account, a women’s daily requirement maybe around 600 IU, that is if she is not deficient and is of an average BMI. If inadequate amounts are taken it can lead to a deficiency that can result in health complications, such as heart disease, fatigue and bone frailty, etc. (Carrelli, A., 2016). One study found that individuals who were undergoing Bariatrics procedures found great benefit from D3 loading under the supervision of a qualified health practitioner, more so if they had fatty liver disease. Bringing up vitamin D serum levels helps to improve mood, improve bone structure, increase energy and regulate metabolism, all of which can benefit an individual in losing excess weight (Luger, M., et al., 2017).
Pollutions Effect on Vitamin D Deficiency
Smog is a potent environmental pollutant that is a combination of fog or haze with smoke often from vehicular exhaust, industrial emissions, etc, as well as dust and soot. Occurring in big cities, where buildings also block sun exposure, smog reduces UV radiation almost by half and significantly more during the afternoon (An, J.L., et al., 2008).
Smog also causes oxidative damage to the skin by reducing vitamin C and E in the top layer of skin (epidermis). These nutrients aid in building collagen and they promote the structure and elasticity of the skin (Thiele, J.J., et al., 1997). Smog has also been shown to increases the build-up of free radical, inflammation as well as changing skin microflora (Mancebo, S.E., et al., 2015).
Poor Kidney and Liver Function
If one’s kidney and liver are not functioning optimally vitamin D cannot be properly processed and activated therefore resulting in a deficiency. Moreover, such a decline in this hormone can also lead to further issues to these organs and other organs. Acute liver fatigue, cirrhosis, hepatic failure, liver cancer can result in a decline in livers’ ability to convert Vitamin D into the active form (Elangovan, H., et al., 2017). To learn more about how poor kidney and liver function affect vitamin D levels, read our article ” Vitamin D and Kidney and Liver Disease”.
Gallbladder Removal
The removal of the gallbladder completely changes the way that digestion functions. Although the liver produces bile, it is stored and released from the gallbladder when digested food or chime moves into the small intestine from the stomach. Without proper bile release, food cannot be properly broken down, which prevents nutrients from being absorbed by the digestive system, this includes vitamin D. To be properly taken up into the body from food sources or supplementation bile needs to be present. Some bile will still be present, as of course it is made by the liver, however, it will not be released promptly when food enters the GI tract, instead, it will slowly trickle in over time.
To enable proper nutrient uptake even without a gallbladder it is recommended to supplement with bile salts with every meal. To learn more consult your qualified health care practitioner.
Cholesterol-lowering Medication Leading to Vitamin D Deficiency
Individuals who take cholesterol-lowering medication can result in a decrease and deficiency in vitamin D. A 2018 randomized, double-blind placebo-controlled study found that vitamin D supplementation taken alongside statin use showed its improvement in effectiveness in long-term use for patients (Wu, Z., et al.). Vitamin D is an integral part of health, statin use, which may be the answer for some individuals who do not discriminate between cholesterol types, therefore when taken vitamin D stores also suffer as they require cholesterol during the process of their activation. Supplementing with Vitamin D will provide positive benefits for those taking statins (Bischoff,-Ferrari, H.A., et al., 2017).
Signs of Vitamin D Deficiency
Vitamin D deficiency is an ignored epidemic, with 1 billion people deficient worldwide, which is about 1 in 8 people. Early signs of deficiency may be very hard to see, even by a physician as it may be masked by bone pain or fatigue. The further from the equator the greater the risk of deficiency, therefore it is important to test serum levels. Deficiency can lead to obesity, diabetes, hypertension, depression, fibromyalgia, chronic fatigue syndrome, osteoporosis, and neurodegenerative diseases. Some studies show that it may contribute to the development of cancers such as breast, prostate and colon as well as having an impact on heart disease, strokes, autoimmune diseases, birth defects, and periodontal disease.
- Rickets in children and the elderly (bow legs, knock-knees)
- Osteomalacia in adults
- Muscle cramping, constipation, nervousness
- Osteoporosis
- Poor bone development
- Colon Cancer and other Cancers
- Heart Disease
- High Blood Pressure
- Autoimmune Diseases (such as osteoporosis)
- Chronic Fatigue
- Allergies
- Asthma
- Psoriasis or eczema
- Recurrent infections
- Infertility – particularly in males
- Depression
Recurrent Infections and Cold
Active D3 is essential in maintaining immune homeostasis and strengthening both innate and active immune response in the body. It does this by targeting several immune cells such as monocytes, macrophages, T-lymphocytes, and B-lymphocytes. A deficiency in D has been linked to a variety of immune disorders (such as cold and the flu), chronic infections and autoimmune disorders (Baeke, F., et al., 2010). D3 has a regulatory effect on gut microbiota and when at optimal serum levels reduces inflammation in the digestive tract. This is important because the gut plays a crucial role in our immune function. If good bacteria is low and inflammation is present our immune function is in peril. Low levels of serum D3 show not only an increase in inflammatory bowel diseases but also in poor immune health (Barbachano, A., et al., 2017).
Increased Chance of Heart Disease and Stroke
Low serum levels of active D3 have been associated with a greater risk of developing cardiovascular disease which can be in part due to calcification of heart valves placing one at risk of a stroke, heart attack or chest pain (angina).
One study found that increased serum levels of active D3 brought about a 15% drop in the development of mitral annular calcification, which is the calcification of the mitral valve ring (Trinaukyy, M., et al., 2017).
Vitamin D deficiency increases biomarkers for cardiovascular disease, more so in women than in men. It elevates the risk of developing myocardial infarction as well as resulting in a greater chance of morbidity in those that already have cardiovascular disease. The reason why vitamin D has such a big impact on heart health is its ability to reduce inflammation, increase insulin sensitivity and reduce/prevent calcification, all of which become issues when serum levels are deficient in active D3 (Fairidi, K.F., et al., 2017) (Lutsey, P.L., et al., 2013).
Development of Osteoporosis and Bone softening
Osteoporosis is the decrease in bone mass and bone tissue leading to a greater susceptibility of fractures. It is most common in aging populations, however, due to lifestyle factors and low active D serum levels it is now seen in younger and middle-aged populations.
Active D3 is crucial to the integrity of the bone structure, mineral metabolism and bringing a balance to bone turnover and growth. Low levels have an impact on bone formation and quality, as the body has to result in stripping minerals (primarily calcium) from bone to compensate for the loss as a result of low D3 levels. Calcium metabolism requires vitamin D to be present otherwise it will not be absorbed into the body from the digestive tract.
Vitamin D is a crucial supplement for individuals with osteoporosis and other bone issues as a preventative measure and to replenish bone with vital minerals and enhance bone growth as well as bone tissue development (Hou, Y-C., et al., 2018) (Lips, P., et al., 2017).
Chronic Fatigue and Low Energy
Low energy and chronic fatigue may be an indication of adrenal strain, which can be made worse by a lack of D3. Although fatigue can occur for a variety of reasons, studies have shown that across the board individuals with fatigue also exhibit low serum levels of vitamin D. It may take some time to rebuild stores and to feel the full effect of supplementation, vitamin D was shown to reverse and prevent the occurrence of fatigue in individuals who experience non-specific fatigue (Johnson, K., et al., 2015).
Low Vitamin D Impact on Sexual Hormones and Erectile Function
A 2017 study found that elevating deficient vitamin D serum levels in middle-aged men improved testosterone levels as well as erectile function. 102 men that participated in the study, age 35-64, had serum levels of less than 30 ng/ml.
Another surprising result was a decrease in BMI amongst the participants. After 12 months of supplementation, serum levels increased to a normal range, then men in the study observed a great positive change (Canguven, O., et al., 2017).
Diabetes and Glucose Sensitivity
A deficiency in vitamin D may lead to complications with the metabolism of glucose and insulin sensitivity. It has been shown to lead to a decrease in insulin release, insulin resistance as well as a contributing factor in type 2 diabetes. One of the ways that a lack of serum active D3 levels can lead to insulin resistance is an increase in inflammatory markers in the body (Lips, P., et al., 2017).
Though supplementing with vitamin D and bringing up serum levels may not reverse diabetes, as there are a lot of other factors that result in the occurrence of the disease, it is important for individuals who have diabetes to bring up active D levels if they are deficient. If one is at risk of developing diabetes and is deficient in vitamin D they must bring up their serum levels as low levels are a contributing factor in the development of insulin resistance and diabetes (Angellotti, E., et al., 2018).
Depression
Depression is a result of changes that occur to one’s neural activity, due to an increase in l-glutamate that increases excitatory neurons and has the potential to lead to a decrease in the activity of GABA inhibitory neurons. The increase in calcium at a cellular level, that often accompanies a decline in vitamin D, contributes to depression and may make individuals more susceptible to developing Alzheimer’s.
This imbalance can be one of many reasons for the commencement of depression. Many other factors can influence and lead to depressive symptoms, such as gut permeability, a permeable blood-brain barrier as well as various nutrients deficiencies. Increasing serum levels of vitamin D aids in bringing balance back to calcium levels in the body which aids in reducing the onset of depression (Berridge, M.J., 2017).
Vitamin D is a crucial nutrient for the human brain. Studies looking at overweight individuals as well as people with chronic spinal injuries have shown a correlation between a deficiency in active D3 levels and depression. Bringing serum levels up has been shown to provide a great improvement and a decline in depression (Murray, M.T., et al., 2012).

Source of Vitamin D
Plant and animal sources of Vitamin D are different, primarily due to the absence of cholesterol in plant sources, which is the main building block of D3 or calcitriol. Although beneficial the conversion to active D3 requires a lot of work on part of the body, therefore if one is not consuming meat supplementing with Vitamin D and getting enough sun exposure is essential in maintaining adequate serum levels.
Vitamin D3: This is found in animal sources and by-products.
The best animal source of D3 is cod liver oil, which is also an excellent source of vitamin A. Free run egg yolks, grass-fed butter, and grass-fed liver are other wonderful sources.
Vitamin D2: Is found in plant leaves – though in a very low amount, moreover as it is in the form of Vitamin D2 it is hard for the body to utilize it and convert it. If an individual is Vegan or Vegetarian it is incredibly important to make sure they supplement with Vitamin D.
Mushrooms and dark leafy greens, such as dandelion greens do contain some D2, though rather low amounts. It is also found in such herbs as alfalfa, nettles, and parsley.
- Cod Liver Oil
- Sardines
- Salmon
- Caviar
- Mushroom
- Mackerel
- Tuna
- Raw Milk
- Eggs (Yolk)
- Beef Liver
- Cheese
|
Food |
Portion |
Vitamin D (I.U.) |
|
Halibut-liver oil |
2 tsp |
9,636 |
|
Herring, grilled |
3 oz. |
850 |
|
Mackerel, fried |
3 oz. |
717 |
|
Cod-liver oil |
2 tsp |
675 |
|
Mackerel, raw |
3 oz. |
595 |
|
Salmon, Pacific, steamed |
3 oz. |
425 |
|
Sardines, canned in oil, drained |
3 oz. |
255 |
|
Tuna, canned in oil, drained |
3 oz. |
197 |
|
Milk, 1% fat |
1 cup |
102 |
Signs of Vitamin D Toxicity
Vitamin D toxicity, also known as hypervitaminosis, is uncommon. Mainly occurring from extensive and excessive over-supplementation. Developing hypervitaminosis from food is very uncommon as very few foods contain such high amounts of vitamin D ( 25(OH)D). Supplementing with 40,000 IU per day over a few months can lead to toxicity as well as a single exceedingly large dosage.
Levels below 30 ng/mL are a sign of deficiency, anything above 150 ng/mL is considered toxic. Though this will vary from individuals to individual age, gender and BMI play a factor in how much serum 25(OH)D is right for you.
Before beginning supplementation, it is always a good idea to test your serum level to know how much you need to take if you are low. When rebuilding your serum levels it is a good idea to retest your levels every month or two to see if your levels have returned to normal and are at optimal levels.
Symptoms of Vitamin D toxicity or hypervitaminosis include the following;
- excessive thirst
- nausea
- diarrhea
- headaches
- weakness
- sunstroke
- vomiting
Testing Blood Levels for Vitamin D Deficiency
The best test is a 25(OH)D test. You can get other tests, such as a ‘1,25(OH)₂D test’, however, the 25(OH)D test will let you know if you are getting enough vitamin D and what your serum levels are.
The optimal levels to strive for at 40-80ng/ml.
Supplementing with Vitamin D
Maintenance levels during times of the years when daylight is at its lowest should be between 2,000 – 4,000 IU per day. D2 (ergocalciferol) and D3 (cholecalciferol) can both be found at supplements, however, to obtain the benefits from calcitriol, it is essential to obtain Vitamin D3.
If one is very low in Vitamin D, is on medication or has certain health conditions it is essential to increase supplementation, for some time, to 10,000 IU daily (no longer than a month at a time, drop to a lower dosage for a month and cycle again, though be sure to test yourself beforehand to see if your serum levels have increased). Smaller dosages will not get your body what it requires and certain conditions will require more supplementation so that the body can convert what it can into an active form (particularly when the issues involve the gut, liver or kidneys). Liquid Vitamin D supplementation is the best and easiest to take. Make sure to check levels for each new season to know when to supplement and when to wain off and enjoy the sun.
When supplementing with Vitamin D it is beneficial to take the supplement with a meal that contains a good amount of fat as the vitamin is fat-soluble. Taking it along with fat will allow for enzymes to be present in the digestive tract to properly ensure the uptake of the nutrient.
Remember to begin with a lower dosage and work your way up. If you are low in Vitamin D, make sure you have also checked the functioning of your liver and kidneys to make sure that they can properly convert vitamin D into its active form of calcitriol in the body. Otherwise, you are going to be paying a whole lot of money for something that won’t be working effectively.
References
An, J.L., Wang, Y.S., Sun, Y., Shen, S.H. (2008). Relationship between surface UV radiation and air pollution in Bejing. Huan Jing Ke Yue. Volume 29, Issue 4, pages 1053-8. Online available at PubMed.
Angellotti, E., David D’Alessio, Bess Dawson-Hughes, Jason Nelson, Robert M Cohen, Amalia Gastaldelli, Anastassios G Pittas; Vitamin D Supplementation in Patients With Type 2 Diabetes: The Vitamin D for Established Type 2 Diabetes (DDM2) Study, Journal of the Endocrine Society, Volume 2, Issue 4, 1 April 2018, Pages 310–321
Baeke, F., Takiishi, T., Korf, H., Gysemans, C., Mathieu, C. (2010). Vitamin D modulator of the immune system. Current Opinion in Pharmacology. Volume 10, Issue 4, pages 482-496.
Barbachano, A., Fernandez-Barral, A., Ferrer-Mayorga, G., Costaler-Carrera, A., Larriba, M.J., Munoz, A. (2017). The Endocrine Vitamin D System in the Gut. Molecular and Cellular Endocrinology. Volume 453, Pages 79-87.
Berridge, M.J., (2017). Vitamin D and depression: Cellular and Regulatory Mechanisms. Pharmacological Review. Volume 69, Issue 2, pages 80-92.
Bischoff-Ferrari, H.A., Fischer, K., Orav, E.J., Dawson-Hughes, B., Meyer, U., Choccano-Bedoya, P.O., Meyer, O.W., Ernst, R., Schitzel, S., Eberli, F., Staehelin, H.B., Freystotler, G., Roas, S., Theiler, R., Egli, A., Wilson, N.M. (2017). Statin Use and 25-Hydroxyvitamin D Blood Level Response to Vitamin D Treatment of Older Adults. Journal of the American Geriatrics Society. Volume 65, Issue 6, pages 1267-1273.
Canguven, O., Talib, R.A., Ansari, W.E., Yassin, D-J., Naimi, A.A. (2017). Vitamin D treatment improves levels of sexual hormones metabolic parameters and erectile function in middle-aged Vitamin D deficient men. The Aging Male. Volume 20, Issue 1, pages 9-16.
Carrelli, A., Bucovsky, M., Horst, R., Cremers, S., Zhang, C., Bressler, M., Schrope, B., Evanko, J., Blanck, J., Siverberg, S.J., Stein, E.M. (2016). Vitamin D Storage in Adipose Tissue of Obese and Normal Weight Women. Journal of Bone and Mineral Research. Volume 32, Issue 2, pages 237-242.
Dowd, J., & Stafford, P. (2008). The Vitamin D Cure. New Jersey: John Wiley & Sons, Inc.
Elangovan, H., Chahal, S., Guton, J.E. (2017). Vitamin D in liver disease in Liver disease current evidence and potential directions. Biochimica et Biophysica Act a (BBA) Molecular Basis of Disease. Volume 1863, Issue 4, pages 907-916.
Eds. Feldman, D., Pike, J.W., & Adams, J.A. (2011). Vitamin D. New York: Elsevier Inc.
ed. Faelten, S. (1988). The Complete Book of Vitamins and Minerals for Health. Rodale: Pennsylvania.
Faridi, K. F., Lupton, J. R., Martin, S. S., Banach, M., Quispe, R., Kulkarni, K., Jones, S. R., … Michos, E. D. (2017). Vitamin D deficiency and non-lipid biomarkers of cardiovascular risk. Archives of medical science: AMS, 13(4), 732-737. Online Available at NCBI.
Holick, M.F. (2010). Vitamin D. Physiology, Molecular Biology, and Clinical Applications. London: Humana Press.
Hou, Y-C., Wu, C-C., Liao, M-T., Shyu, J-F., Hung, C-F, Yen, T-H., Lu, C-L., Lu, K-C. (2018). Role of Nutritional Vitamin D in Osteoporosis treatment. Clinica Chimica Acta. Volume 484, pages 179-191.
Johnson, K., & Sattari, M. (2015). Vitamin D deficiency and fatigue: an unusual presentation. SpringerPlus, 4, 584. Online Available at PubMed.
Kennel, K. A., Drake, M. T., & Hurley, D. L. (2010). Vitamin D Deficiency in Adults: When to Test and How to Treat. Mayo Clinic Proceedings, 85(8), 752–758.
Khalsa, S. (2009). The Vitamin D Revolution. United States: Soram Khalsa.
Lips, P., Goldsmith, D., de Jough, R. (2017). Vitamin D and osteoporosis in Chronic Kidney Disease. Journal of Nephrology. Volume 30, Issue 5, pages 671-675.
Luger, M., Kruschitz, R., Kienbacher, C., Traussingg, S., Langer, F.B., Prager, G., Trauner, M., Krebs, M., Marculescu, R., Ludrik, B. (2017). Vitamin D3 Loading is Superior to Conventional Supplementation After Weight-loss Surgery in Vitamin D-deficient Morbidly Obese Patients: A Double-Blind Randomized Placebo-Controlled Trial. Obesity Surgery. Volume 27, Issue 5, Pages 1196-1207.
Lutsey, P. L., & Michos, E. D. (2013). Vitamin D, calcium, and atherosclerotic risk: evidence from serum levels and supplementation studies. Current atherosclerosis reports, 15(1), 293. Online available at PubMed.
Mancebo, S.E., Wang, S.Q. (2015). Recognizing the impact of ambient aid pollution on skin health. Journal of the European Academy of Dermatology and Venereology. Volume 29, Issue 2, page 2326-2332.
Murray, M.T., Pizzorno, J. (2012). The Encyclopedia of Natural Medicine. Atria: New York.
Naeem, Z.(2010). Vitamin d deficiency- an ignored epidemic. International journal of health sciences, 4(1), V-VI. Online Available at NCIB.
Norman, A.W. (1979). Vitamin D. The Calcium Homeostatic steroid Hormone. New York: Academic Press, Inc.
Perez-Lopez, F.R., Brincat, M, M., Erel, T., Tremollieres, F., Gambacciani, I., Lambrinoudaki, I., Moen, M.H., Schenck-Gurtafsson, K., Vujovic, S., Rozenberg, S., Rees, M. (2012). EMAS position statement: Vitamin D and Postmenopausal Health. Maturitas. Volume 71, Issue 1, pages 83-88.
Thiele, J.J., Traber, M.G., Tsang, K., Cross, C.E., Packer, L. (1997). In vivo exposure to Ozone Depletes Vitamin C and E and Indices Lipis Peroxidation in Epidermal Layers of Murine Skin. Free Radical Biology and Medicine. Volume 23, Issue 3, page 385-391.
Tribuakuu, M., Zhao, D., de Boer, I.H., Guallar, E., Bortnick, A.E., Lutsey, P.L., Budoff, M.J., Kizer, J.R., Kestenbaum, B.R., Michos, E.D. (2017). Relation of Serum Vitamin D to Risk of Mitral Annular and Aortic Valve Calcium (from the Muti-Ethnic Study of Atherosclerosis). The American Journal of Cardiology. Volume 120, Issue 3, pages 473-478.
Tripkovic, L., Lambert, H., Hart, K., Smith, C. P., Bucca, G., Penson, S., … Lanham-New, S. (2012). Comparison of vitamin D2 and vitamin D3supplementation in raising serum 25-hydroxyvitamin D status: a systematic review and meta-analysis. The American Journal of Clinical Nutrition, 95(6), 1357–1364. Online available at PubMed
Wu, Z., Camargo, C.A., Khaw, K-T., Waayer, D., Lawes, C.M.M., Toop, L., Scragg, R. (2018). Effects of Vitamin D supplementation on adherence to and persistence with long-term statin therapy: Secondary analysis from the randomized, double-blind, placebo-controlled ViDA study. Atherosclerosis. Volume 273, pages 59-66.
Amanda Filipowicz is a certified nutritional practitioner (CNP) with a bachelor in environmental studies (BES) from York University. She also has certification in clinical detoxification, prenatal and postnatal care as well as nutrition for mental health. She has been working as a nutritionist since 2013 and is a lifelong proponent of eating healthy.

