Our bodies have an entire universe of microscopic organisms living inside of it, many of them are good, some are bad, and when the balance gets out of hand the dark side often wins out (dysbiosis) but there are many things you can do about it. There are no quick fixes, you can take medication or creams, but as you probably know your self, the culprit comes back with a vengeance. Vaginal yeast infections affect all women, as you may have seen in magazine articles or videos, think of a woman a celebrity, royalty, your neighbor and that woman has probably had a yeast infection. I have had yeast infections (yes, that is a plural). It has been quite some time since I last had one and it is mainly because I finally know how things are run down there and I take a lot of care to make sure it is at its best health all the time.
What is a Yeast Infection
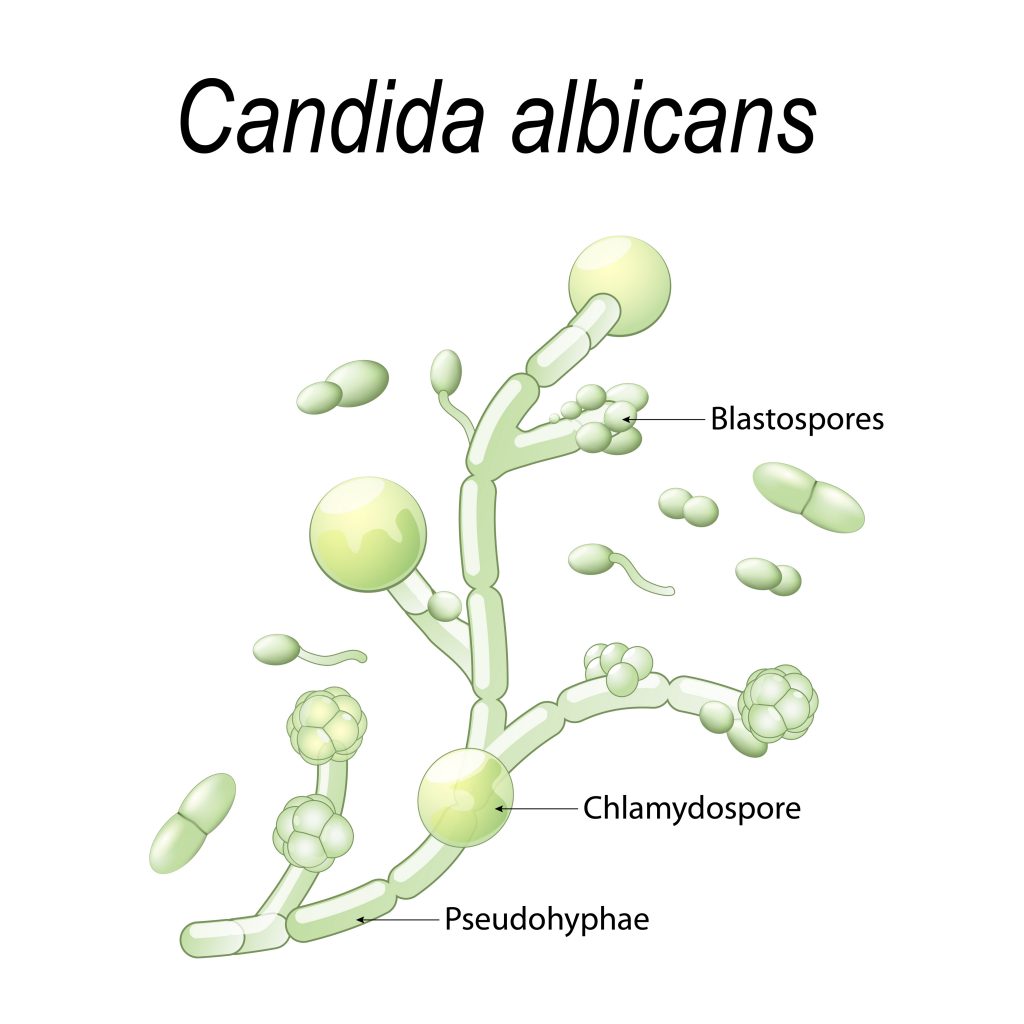
Yeast is a microscopic organism that is categorized as a fungus (polymorphic fungus), the most common yeast in the body is Candida albicans, though it is not the only species of candida present (Greenfield, B., 2014). Candida naturally exists as part of the healthy human microbiota, colonized within the digestive system (primarily the large intestine) and smaller colonies in the mouth and genitalia (ed. Prasad, R., 2017). It mainly exists to eat away at heavy metals that make their way into the body, therefore, they do have a good and effective purpose in the body, it is when their growth in the moist mucous membranes becomes out of hand and begins to change the ecosystem of our bodies that candida is an issue (Rapp, D., 1991).
Candida is an opportunistic infection, it affects both men and women and can be passed on to your partner. Candida does not work alone, it shares a biofilm with bacteria and parasites, allowing these three opportunistic organisms to rapidly multiply and wreak havoc on the walls of the digestive tract (Junger, A., 2013). Mucosal diseases such as a vaginal yeast infection can arise, however, the effects of candida overgrowth can sometimes become life-threatening, particularly in individuals who have impaired immune function (ed. Prasad, R., 2017).
Vaginal Infections often arise as a result of antibiotic use, over-consumption fo sugar or bad hygiene. Candida which is often suppressed from overgrowing by healthy gut bacteria is now able to grow rapidly as much of the beneficial microflora is whipped out as a result of antibiotics (unless it is repopulated through supplementation), outbalanced because the bad bacteria feed on excess sugar or as a result of pH imbalances. Yeast produces an excess toxic waste that can travel via the blood and affect the body as a whole leaving you feeling ill, tired, often craving sugar and carbs and leave you feeling itchy and inflamed (Rapp. D., 1991). 75% of women of reproductive age will experience at least one yeast infection in their lifetime. 40-45% of these women will have recurrent infections (at least 2 or more), an increase since the 90’s when the rate of recurrence was approximately 5-10% of women. Candida albicans represents 90% of yeast infection in the United States (ed. Prasad., 2017) (CDC, 2017).
A yeast infection is diagnosed as a microscopic identification of a large cluster of yeast cells on the vaginal smear, as well as a physical examination of symptoms, such as white discharge from the vagina, localized itching and irritation and inflammation of the vagina (Cribby, S., et al., 2009). Although some tests for yeast infections may come back stating that there is a very low presence of healthy bacteria (which is often the case with individuals who have been taking antibiotics) it is not always the case. Lactobacilli bacteria are still sometimes found in individuals with yeast infections (ibid). This is often due to the reason for the infections, such as high sugar consumption, poor dietary choices, bad hygiene, or even high stress.
Vaginal Yeast Infection Causes
Candida as said before is an opportunistic organism, since the 1940s with the introduction of antibacterial antibiotics as a medicinal therapy, there has been an ever-increasing issue of serious candidal infections in individuals who have used antibiotics (ed. Prasad, R., 2017). There are numerous other reason for Candida overgrowth – or vaginal yeast infection – that we will get into in this section, it is important to understand that it is usually a combination of issues that lead to a yeast infection, some being more prevalent than others. Each individual is unique and it is hard to pinpoint that this one thing is what is causing a yeast infection in your body, however, one of the most important things to look at is your digestive health and what you put into your body. Feeding bad bacteria and creating an environment for it to thrive is not going to prevent infections even if you take antibiotics or medication. It is important to grow healthy bacteria colonies and feed the good bacteria while starving the bad guys so they can’t wreak havoc.
There are six main causes of vaginal yeast infections;
- Antibiotic Use
- Bad Hygiene
- Poor Immune Systems
- Poor digestive health
- Sexual Intercourse
- Toxins and Heavy Metals
To learn more details about what causes a Vaginal Yeast Infection read our 6 Causes of a Vaginal Yeast Infection Article.
Antibiotic Use
Antibiotic use not only eliminates bad bacteria but the good as well. If good bacteria is not reintroduced and rebuilt after antibiotic use, candida can build up and lead to a vaginal yeast infection.
Bad Hygiene
The vagina is a self-cleaning organism with a low pH. The use of soap, sprays and perfumes can have a negative impact on the health of the vagina, making it susceptible to infection. If you are experiencing bad odours, it is best to address the issue (most likely a vaginal imbalance or a vaginal yeast infection) instead of covering it with perfumes, creams and sprays.
Wearing cotton underwear, only using clean water to cleanse your vagina, not always wearing tight fitted pants, consuming a wholefood, alkaline diet are all things that you can do to maintain a healthy vagina.
Immunocompromised Individuals
People with poor immune systems are more susceptible to developing infections. Often they also have poor gut health, which leads to an increase in bad bacteria development and candida overgrowth. Many immunocompromised individuals consume pain medication, antibiotics and cold and flu medication, all of which can greatly affect the health of the microbiota. A traumatic situation or event can also result in vaginal yeast infections as they negatively affect the microbiome and other organs of the body.
Poor Digestive Health
The vagina is an echo of your digestive health, and the digestive system is a mirror image of the health of the entire body. If your digestive system is compromised, if it is constantly inflamed, susceptible to SIBO, permeability and fostering a lot of bad bacteria, likely, your vaginal health will not be very good, and it can lead to a vaginal yeast infection.
One of the most problematic things that we place into our diet and digestive system that feeds candida uncontrollably is sugar.
Sexual Intercourse
Sexual activity has been shown through many studies to increase the pH of the vagina and possibly result in a vaginal yeast infection or other infections of the vagina. Having unprotected sex drastically reduces the count of healthy bacteria in the vagina, mainly attributed to the act that semen has an alkaline pH (Jespers. V., et al., 2015)
Toxins and Heavy Metals
High mercury levels in the body can result in candidiasis overgrowth in the vagina (as well as other areas of the body) – which can lead to a vaginal yeast infection. Mercury salts not only feed and allow bad bacteria or yeast to thrive, but it also prevents the growth of good bacteria in the gut and vagina.
Vaginal Yeast Infection Symptoms
You will know that there is sometimes not quite right down there when you have a vaginal yeast infection, it is going to be uncomfortable and nothing you do will provide any comfort.
- Vaginal itching and soreness
- Pain during sexual intercourse
- Pain and or discomfort when urinating – due to sore tissue
- Abnormal vaginal discharge – cottage cheese-ish – odourless
- Swelling (irritation and inflammation) of the vagina
(Cribby, S., et al., 2009)
Yeast Infection Symptoms
Sometimes you may be able to catch a yeast infection before it starts to spreads throughout your body. Candida, that naturally lives in the digestive system, cleanses the body of heavy metals but when it begins to overgrow it starts to wreak havoc. This havoc can be felt like the symptoms listed below. These symptoms can also be felt when you have a vaginal yeast infection, though they pertain to yeast infections as a whole. The five symptoms listed above are particular to a vaginal yeast infection.
- White coating on the tongue
- Digestive issues – constipation, bloating, gas
- Depression, irritability and anxiety
- Can’t-lose weight
- Mental fog
- Chronic fatigue
- Sugar and carb cravings
- Chronic sinus/excess mucus
- Dry, itchy skin, eczema/psoriasis
- Nail or toe fungus
- Food and/or environmental allergies
The toxins produced by candida are thought to affect the area of the brain that is in control of mood and outlook, often leading to feelings of depression and anxiety.
Yeast overgrowth weakens the immune system leading children and adults to become prone to infection. The mucus lining of the digestive tract weakens resulting in an increase of toxic bacteria that enters the bloodstream and leading to issues of the nervous system (Rapp, D., 1991).
A Healthy Vagina
To understand what can go wrong with your vagina and how to turn back the tide on yeast overgrowth or a yeast infection it is important to know how a healthy vagina should feel and function. The vagina is mainly colonized by lactobacillus bacteria and it is this good bacteria that suppress pathogenic bacteria and yeast. Lactobacillus bacteria provide both lactic acid and hydrogen peroxide, making it a great and powerful defence against bad bacteria and other unwanted invaders into the vaginal canal, such as yeast. However, it needs to be well taken care of so that it can thrive (ed. Schlossberg, D., 2008).
The production of hydrogen peroxide by lactobacillus and lactobacillus’ metabolic end product lactic acid is responsible for fending off foreign invaders and for maintaining a healthy ecosystem in the vagina – an acidic ecosystem. The vaginal ecosystem is much more acidic than blood or intestinal fluids, it needs to be that way, just like our mouths do, to kill off any bacteria, fungus or other foreign particles that come in (Linhares, I.M., et al., 2011) (Brunzel, N.A., 2018).
How acidic does the vagina need to be to be considered healthy? A neutral environment is present at a pH of 7, a healthy vagina will produce secretions in the range of 3.8 to 4.5 pH. Anything higher than 4.5 pH will often result in a yeast infection, bacterial vaginosis, atrophic vaginitis or trichomoniasis (Brunzel, N.A., 2018). Without Lactobacillus present, as well as a few other factors the pH of the vagina will not stay as acidic as it should and will begin to grow more alkaline making it the perfect breeding ground for bad bacteria and yeast. Therefore, it is very important to make sure that lactobacillus bacteria maintain dominance in the vaginal ecosystem (ed. Schlossberg, D., 2008).
The most dominant type of Lactobacillus is Lactobacillus crispatus. It produces a high amount of hydrochloric acid (H²O²) to help prevent the overgrowth of anaerobic bacteria and is present in concentrations of 10⁶ bacteria by ml of vaginal fluid (ed. Schlossberg. D., 2008). Lactobacillus vaginalis is another very important player in a healthy vagina. This species of Lactobacillus is also present at a high amount in a healthy vagina, also amount 10⁶ bacteria per ml of vaginal fluid. However, in a 2007 study published in the Journal of Applied Microbiology, it was shown that there are microbiological differences in the vaginas of different ethnic and cultural groups (Jespers, V., et al., 2015). Women from Uganda and Korea were observed and it was found that women from Uganda possessed Lactobacillus vaginalis were as Korean women did not (instead they had Lactobacillus fermentum – which women of Uganda did not carry). L. crispatus and L.vaginalis are not the only two bacteria that produce lactic acid (they are simply present at high concentrations and L.crispatus is seen in the vaginas of most healthy women on the planet), Leuconostoc, Pediococcus (all strains from this genera inhibit Candida species), Streptococcus and Weissella also have species among them that aid in the production of lactic acid and prevent the spread of pathogenic bacteria and yeast (Jin, L., et al., 2007).
A healthy vagina will not display foul odours, burning sensations, discomfort or unnatural discharges (usually of white or grey colour – this is a sign of a vaginal yeast infection) (ed. Schlossberg, D., 2008). It also requires the presence of hydrogen peroxide producing bacteria. Even if there are other healthy bacterial colonies present in the vagina if hydrogen peroxide is not being produced, you will be susceptible to developing a yeast infection or other bacterial infections of the vagina (Stephen, E.H., et al, 1996).
Healthy Bacteria That Colonizes The Vagina
50 different strains of healthy bacteria are found within the vagina (comparable to the gut that can have approximately 800 distinct strains). The reasons for such low probiotic counts within the vagina may be a result of poor nutritional availability for the bacteria present as well as competition with indigenous organisms (Cribby, S., et al., 2009). Lactobacillus species accounts for between 50-90% of healthy vaginal microbes. The most common Lactobacillus species found in the vagina include the following, L.iners, L.crispatus, L.jenesenii and L. gasseri. The second most common ones include L.acidophilus, L.plantasrum, L.fermentum, L. brevis, L.vaginalis, L.casei, L.delbrueckii, L.salivarius, L.rekteri and L.rhamnosus (ibid). When selecting a probiotic supplement to take for increasing healthy vaginal flora it is best to make sure that it includes some if not many of these strains.
L.crispatus is a strain of bacteria that produce hydrogen peroxide in the vagina. It is beneficial in preventing BV infections and aids in keeping the vagina clean of foreign pathogens. Not found in all women, though present in North America, Europe and Japan.
L.iners another bacterial strain of a healthy vagina, however, it has also been detected during vaginal dysbiosis. It has recently been detected as a species of vagina bacteria therefore, not much is known about it.
L.gasseri strain of bacteria has potent antiviral activity, particularly against herpes simplex type 2. Naturally found in a healthy vagina.
L.jenesenii a strain of bacteria isolated from the vaginas of healthy females. Produces hydrogen peroxide. Protective against infections, particularly bacterial vaginosis.
Different Species of Candida
The increase in candida overgrowth and related illnesses is due to our medical practices and the species that infect the body are dependant on infection site and geography. 92-95% of all infections are a result of C.albicans, C.glabrata, C. parapsilosis, C.tropicalis and C.krusei, Candida albicans accounting for more than 50% of all infections. In the USA C.glabrata is the second most common yeast growth, followed suit by C.tropicalis and C.parapsilosis. In the past few decades, non-Candida albican species of infections have been on the rise as many have an inherent resistance to antifungal medication, such as C.auris which has a multi-drug resistance of 93% comparable to C.albicans which has a resistance of 0.5-2% or C.tropicalis and C.parapsilosis which have a resistance range of between 4-9% and 11-13%(Berkow, E.L., et al., 2017).
Candida albicans is the most common form of candida that resides within the body. It can be found naturally colonized in various areas of the body, such as the gastrointestinal tract as well as the genital and urinary organs. Increased levels of stress, lowered immunity, a change in the microbiology of the body and other factors can result in the overgrowth of this yeast – leading to infection and illness (Nobile, C. J., & Johnson, A.D., 2015).
Candida glabrata a small percentage of vaginal issues such as yeast infections is caused by this strain of candida (eds. Sweet, R.L., et al., 2009). It is most common in North America, and Northern Europe primarily causing vulvovaginal candidiasis (Whaly, S.G., et al., 2016). It was until recently considered a nonpathogenic fungus. The use of immunosuppressant drugs (medications for psoriasis, lupus, autoimmune arthritis, etc) as well as systemic infections results in increased growth of C.glabrata. This species of candida also has resistance to certain medications that would normally treat candida (Fidel, P.L., et al., 1999). It is particularly prevalent among individuals suffering from diabetes (Whaley, S.G., et al., 2016).
Candida krusei is common in patients with hematologic malignancies (a form of cancer) as well as individuals who have received an organ transplant. It is seen as a potentially drug-resistant yeast agent (Pfaller, M.A., 2008) as it has a natural resistance to fluconazole (Berkow, E.L, et al., 2017). North America, globally more susceptible to this disease, whereas South America is far less susceptible (this could as with other infections) be dependant on the differing bacterial ecology (Pfaller, M.A., 2008).
Candida parapsilosis is becoming a major cause of vaginal and digestive dysfunction (Trofa, D., et al, 2008) and is becoming an issue amongst the pediatric population affecting infants and neonates with fungal growth (approximatly 17-50% of fungal growth in infants is caused by this form of candida) (Whaley, S.G., et al., 2016). Yet again, this form of Candida is very prevalent among individuals who are immunocompromised. patients with prosthetic limbs, catheters are more likely to contract an overgrowth of this Candida species. It mainly grows on human skin, making it easily spread by hands and thus throughout hospitals if patients and practitioners do not practise proper hygiene (Trofa, D., et al., 2008).
Candida tropicalis has become a growing cause of infections in the body. It is most common in South Pacific Asia where it is responsible for approximatly 20-45% of Candida infections. It is also responsible for a very high mortality rate amongst the elderly in South Pacific Asia approximatly 30-70% (Whaley, S.G., et al., 2016). It is resistant to fluconazole (an anti-yeast.fungal medication effective against Candida albicans). It is close to C. albicans taxonomically and shares many of its traits, such as creating a biofilm (a protective coating that shields the yeast from our immune system) (Zuza-Alves, D.L., et al., 2017).
Vaginal Yeast Infections and the Pill
The birth control pill affects the ecology of the vaginal region as well as imbalances hormone levels in the body. The pill increases estrogen levels, along with birth control patches and rings, which over time leads to an overgrow of yeast in the vagina (and gut) (Chia, M., & Abrams, R.C., 2006). Furthermore, levels of glycogen (a type of sugar) increase in vaginal secretions further feeding yeast and bad bacteria and resulting in its overgrowth – which could potentially lead to a vaginal yeast infection. (Ross, J., 2012).
The birth control pill depletes vitamins B2, B6, B12, C, E, folic acid, magnesium and zinc as well as coenzyme Q10. If you wish to continue to take birth control pills it is best to take a high potency multivitamin as well as chlorophyll or another alkalinizing supplement.
Other contraceptive products such as spermicidal creams and forams contain the active ingredient nonoxynol-9. This ingredient lowers the body’s immune system and destroys beneficial lactobacillus colonies in the vagina leaving the vagina more susceptible to developing a vaginal yeast infection or even E.coli overgrowth (Ross, J., 2012).
Vaginal Yeast Infection during Pregnancy
The high levels of estrogen and progesterone that accompany pregnancy are associated with yeast infections (Chia, M., & Abrams, R.C., 2006). However, it is also common for pregnant women to experience a normal discharge of a mild smelling milky substance from their vaginas. One should never try to self-diagnosis, especially not when one is pregnant, it is always best to seek an expert opinion (or two or three). This natural discharge increases as one comes to term. It is often comfortable to wear a pad, however, refrain from using tampons as they have a high likelihood of resulting in infection (Murkoff, H., et al., 2002).
Candida is slightly more difficult to eradicate for the vagina during pregnancy. The Center for Disease Control recommends pregnant women take a topical cream such as clotrimazole, miconazole, butoconazole or terconazole for a period of seven days. However, it is also beneficial before trying these creams out to try a holistic approach (eds. Sweet, R.L., Gibbs, R.S., 2009). Concerning alternative treatments do not douche, it’s not a good idea when you are not pregnant and definitely, a bad idea when you are at it can result in BV, other vaginal infections and even a preterm birth (Murkoff, H., et al., 2002).
Vaginal Yeast Infections and PMS
Just as the pill and pregnancy can cause yeast infections so can our menstrual cycle. This is not for all women, but for those who experience very bad mental pain and PMS symptoms their hormones can be really out of wack and they can sometimes have abnormally high levels of estrogen (Chia, M., & Abrams, R.C., 2006).
If you have bad PMS symptoms, particularly sugar cravings, this can also add to an increased susceptibility of a yeast infection. Consuming high amounts of sugar, combined with fluctuating hormone levels (estrogen and progesterone) can lead to a yeast infection. The use of tampons that do not contain organic cotton can also negatively affect the vaginal environment as many contain pesticides, toxins, bleaches etc. The use of soap down there can also change pH balance (making it more alkaline). The vagina is a self-cleaning organ, it doesn’t need any soap. If it’s smelling a little funky down there, go see a doctor get a diagnosis as it can be a sign of bacterial vaginosis or a vaginal yeast infection. Use water and that’s it. If you need a little extra cleaning dry brushing will help get rid of dry skin and aid in exfoliating.
Vaginal Yeast Infection Treatment
Lifestyle changes, involving diet, daily habits, etc are the easiest things to implement to prevent the spread of yeast in the body, eliminate it and stop recurrent yeast infections from occurring. Medications applied as suppositories, creams or taken orally can be effective, however, it is being seen more and more often that different strains of candida have a resistance to them or when taken the yeast infection becomes recurrent.
Providing the body with a fighting chance against pesky yeast will make it easier for yeast overgrowth to be suppressed and infections will not happen in the first place. Boosting the immune system, providing the digestive system with diverse beneficial bacteria, reducing sugar consumption and practising good hygiene will all aid in preventing vaginal yeast infections naturally.

Dietary Changes During A Vaginal Yeast Infection
Sugar in all its forms is the first thing that needs to go. This means fruits too. We hear that it is important to eat mostly plants, fruits are plants, but they are also packed with sugar (Junger, A., 2013). Now the sugar in fruits is so much better than the processed corn, beet or cane sugar that is found in many sweets and prepackaged meals. But no matter its form, sugar feeds candida. Consuming it only adds to the chronic situation in your vagina. It is a little difficult at first and you may experience some withdrawal symptoms but with the time you will feel so much better, far better than you ever remember feeling. dried fruit and bananas have a lot of sugar in them, as do ripe fruits. Chocolate, sweets, ice cream, for the time being, need to leave. If you do experience cravings, including a good source of fat in the diet, fibre such as flax seeds and cinnamon all aid in balancing blood sugar levels.
Some fruits can be included in the diet, these include green apples, pomegranates, lemons and limes avocados (also a great source of fat) and all berries. Making sure that they are organic and local when you can. Some pesticides, herbicides and other chemicals can have anti-fungal, anti-yeast activity in the body, thus though they may do away with the bad, they do away with the good as well.
Other foods that should be excluded from the diet because of their either aid in the growth of candida, or mucous formation includes;
- coffee
- black tea
- dairy (goat cheese may be okay, but it is preferable to exclude it during the process of eradicating candida from the body)
- soy
- corn
- allergens/foods you are intolerant to
- wheat
- nightshades
Many of these foods, when the digestive system is suffering from dysbiosis, the immune system is low and candida is overgrowing, not just the vagina but also the gut, which can cause serious problems. When the body is balanced, and the immune system is functioning optimally, if nightshades are ingested inflammation will be suppressed and it won’t be an issue. However, if the immune system is having trouble suppressing candida overgrowth, it will not have the strength to also suppress inflammation. The same can be said for dairy products and wheat, which are mucus-forming, coffee that speeds up digestion (we want to improve digestion and the secretion of juices, such as pancreatic acid which also aids in the elimination of candida), and allergens of intolerant foods that inflame the digestive tract.
Mushrooms should also be limited during this time. though some mushrooms have amazing healing properties for the digestive system, they still have a high likelihood of continuing mould, and mould feeds candida. This can also be said for peanuts and pistachios, both of which have a high probability of mould (no peanut butter either).
Fermented Foods
Fermented foods (aside from alcohol) feed the digestive system with healthy bacteria, however when there is dysbiosis present in the body instead of feeding and repopulating beneficial flora it feeds and aids int eh growth of bad bacteria and yeast. Yeast loves to munch on fermented foods. There are times when whole foods are beneficial but when the body is out of balance it is important to replenish missing nutrients and bacterial flora with supplementation. Fermented foods to avoid include;
- yogurt
- alcohol
- kombucha
- saurekraut
- kimchi
- apple cider vinegar
- miso
- natto
- soy sauce
- sourdough bread
- kefir
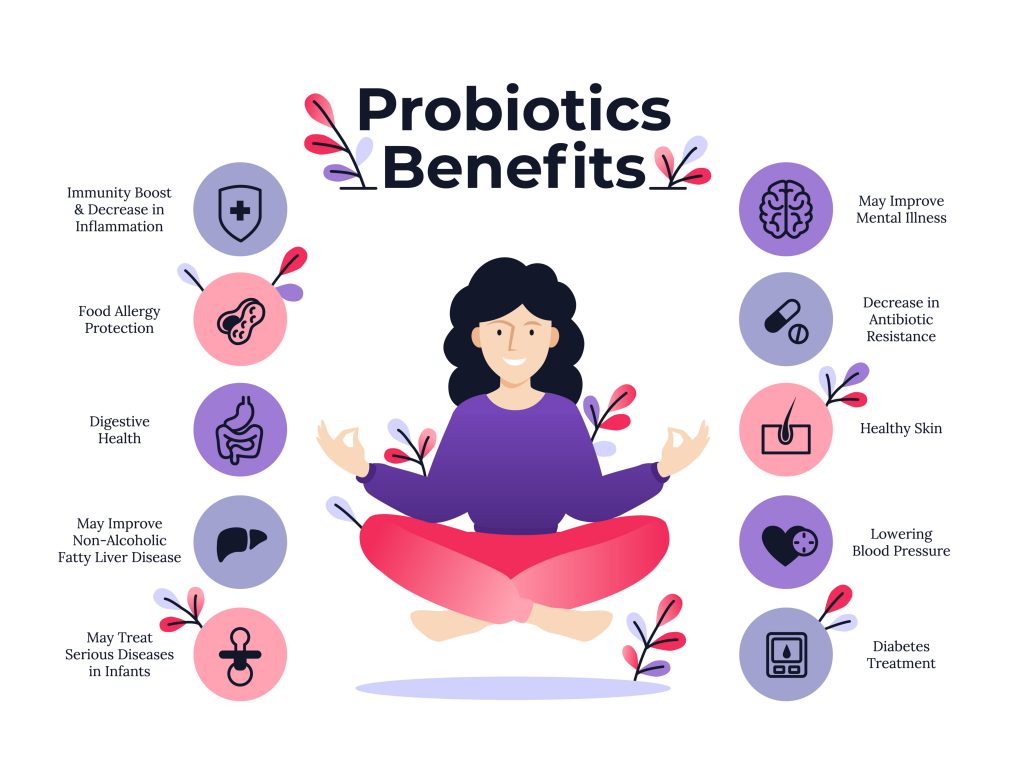
Probiotics
We want to eliminate the bad bacteria, at the same time replenishing the counts of healthy bacterial populations in the vagina. Probiotics are best taken with food and away from any antifungals, antibacterials, this includes herbs and natural health products.
When you are cleansing the body of yeast, as is stated above you do not want to consume any fermented foods. Although it is important to naturally enhance the bacterial colonies in the body, we want to suppress yeast growth and provide the digestive system and the vagina with natural fighters to further aid in the elimination of the infection.
Providing the body with a high potency probiotic orally and a vagina suppository probiotic can quickly and effectively rebalance healthy bacterial populations and begin to revert dysbiosis. To learn more about probiotics, their benefit for the body and which ones to take, click over to our probiotic article.
Anti-yeast Foods
Unfortunately, there are many foods that need to be avoided so as to eradicate candida from the vagina and body. However, there are also delicious foods that can be added in or their consumption increased as they aid in the elimination of yeast from the body. These include broccoli, horseradish, kale, turnips, and cabbage (Rapp, D., 1991).
Garlic
Garlic is great at fighting against vaginal yeast infections. It is a natural anti-fungal, anti-inflammatory and it boosts up the immune system. Eating 1-2 raw cloves of garlic can be very beneficial for both yeast infection prevention and fighting one-off. Throwing raw garlic into salad dressing, mixing it in with quinoa or adding it to a soup. Supplementing with garlic capsule can also be very effective, a recommended dosage is approximately 900mg (Stone, J.J., 2015). Even cooking or roasting garlic can still be effective against the suppression and spread of yeast in the body, you might just need to eat a little more.
Papaya
Papaya has numerous health benefits, one of them being an anti-yeast activity, particularly against Candida albicans, Candida guilliermondii and Candida tropicalis – which can help during the treatment of yeast infections. (Arvigo, R., & Balick, M. J, 1993).
Sage
This delicious herb that is often paired with meats, fish and root vegetables or adorned on pasta is also a very potent antibacterial and fungistatic. Sage also presence astringent, and virostatic actions on the body. Boosting the immune system with its compound phenolic glycoside which is a potent antioxidant and supporter or a healthy mucosal lining in the body and vagina (Lezak, M., 2000).

Lifestyle Changes for a Vaginal Yeast Infection
There are many things that you can do to prevent the overgrow of candida in the vagina and also aid in the elimination of a vaginal yeast infection. One of the most important things to remember is to keep the vagina dry, on a daily bases and during menstruation. After you have used the washroom, pat yourself down well, though not vigorously. If you have your period make sure you do the same and change your pad or tampon as soon as it can’t hold any more liquid (Batra. S., 2003) (Chia, M., & Abrams, R.C., 2006).
Refrain from wearing tight underwear or clothing and wear cotton underwear. This is one you hear a lot. Yoga pants can be very comfortable, but they are also rather tight fit and not all of them are made from a material that absorbs moisture or is breathable. Lacy underwear is often not made of cotton, though just because you wear it does not mean that you will get a yeast infection, nor if you hang out in your yoga pants day in and day out. If you happen to have a yeast infection, wearing lacy undergarments and yoga pants, pantyhose, tight jeans, shorts or pants may not be the best solution, you want your vagina to breathe. Be mindful of your body, if you need to go to work dressed a certain way, as soon as you come home to loosen up and let everything breathe. A great tip is to let your vagina breathe at night, wear a nightdress (with no underwear) or nothing. Here are some other lifestyle tips:
Don’t wear panty liners every day, they hold a lot of moisture which in turn moistens the vagina. However, if you happen to have a yeast infection and you are on your period do use pads. Tampons will hold moisture in the vagina as well as the infection (Stone, J.J., 2015). Remember menstruation is a way for the body to cleanse, therefore, with your period some of the yeast and bad bacteria will be eliminated as well.
If you wash your fancy undergarments by hand, don’t overdo the detergent. Even if you are using a washing machine or cleaning service, make sure that the detergent is as natural as possible and free of harmful chemicals and perfumes (The Honest Compay has a very nice selection of laundry detergents). It is best to go with an all-natural detergent one that is appropriate for sensitive skin (the skin is sensitive down there) and that contains no perfumes. if you would like your clothing and underwear to have a nice scent add some organic essential oils such as lavender during the washing process. Or add lavender and essential oil sachel into your closet or drawer to naturally freshen and scent your clothing.
Stress is never a good thing for the body high amount of stress can cause bad bacteria to overgrow and leaving a pathway for candida to take up residence where it is not wanted. Stress can also steer us into bad cravings for sugary goods – feeding the little candida you have in your body and giving it the strength to grow. Stress, when it gets out of control, can also affect our immune system. The immune system daily, when it is functioning optimally, can combat candida if it begins to get out of control if the immune system is weak it will not be able to suppress candidal overgrowth (Stone, J.J., 2015).
Sleep is essential for the body to heal. Good quality sleep restores the immune system and allows it to clean house. If you are lacking good quality sleep due to insomnia or waking up several times a night, your immune system will begin to wear down and a weak immune system will not be able to suppress candida overgrowth when it occurs. To learn more about how to improve your sleep habits check out our Why is Sleep Important? post!
Vaginal Yeast Infection Creams and Medication
In the 1990’s antifungal medication became available over the counter. Approximately 73% of women with chronic vaginal symptoms use over the counter medication. However, self-diagnosing and self-treatment with such medication can be harmful – since most of the time women misdiagnose themselves (symptoms may be pertaining to a more serious issue) and though the medication takes away symptoms they do not cure the underlying issue. Besides, antibiotic use is one of the leading causes of yeast and other vaginal infections (Beigi, R.H., et al., 2004).
You can take oral and topical medication, however, they do not deal with the underlining imbalances in the body. Sometimes medication can aggravate the issue (Mindell, E., 2004). Failure of Yeast Medications and/or creams and the recurrence of Vaginal Yeast Infections are very common (eds., Sweet, R.L., et al., 2009), as the medication is simply removing the symptoms and not solving the issue.
Antibiotics not only decrease bad bacteria but good bacteria as well. Over time, if not repopulated and properly taken care of can lead to a decrease in B12 and folic acid production within the digestive system. Therefore, if you are planning on using over the counter medication or antibiotics make sure to repopulate the digestive system and the vagina with good bacteria and support their development with a healthy alkalinizing, anti-inflammatory and sugar-free diet. The use of intravaginal probiotic suppositories, as well as probiotic supplements, will be beneficial in restoring a healthy gut ecosystem and allowing it to thrive as suppressing the recurrence of unwanted bad bacteria and yeast.
Antifungal Medication
If you are being treated for a vaginal yeast infection with antibiotics/antifungals orally or intravaginally you will very likely contract a yeast infection again if the healthy bacteria in your digestive system is not re-colonized (Mindell, E., 2004). Many of us take them without later supplying our digestive system with the nutrients and healthy microbes that it needs to properly function leading to future repeat infections. However, this is not the only problem that antifungals pose. Many antifungal medications are made to combat Candida albicans alone, be that as it may, more individuals are experiencing candida overgrowth that is caused by non-albican candida species – many of which are resistant to antifungal medication (Sanguinetti, M., et al., 2015).
Fluconazole
Fluconazole is the primary therapeutic option for North America and Europe (Berkow, E.L., et al., 2017) and is the most commonly prescribed antifungal drug. It works by inhibiting ergosterol (a compound found in the fungal cell membrane) biosynthesis, thus preventing the fungal cell from growing or multiplying (Berkow, E.L., et al, 2017). It is known as an azole antifungal agent and is preferred for its inexpensiveness, limited toxicity and oral administration (Whaley, S.G., et al., 2016).
This antifungal medication is used to combat Candida infections of the vagina, mouth and throat (Martino, M.D., 2011). It does not have any known interactions with herbal or nutrients, nor is it known to displace nutrients within the body (eds. Gaby, A.R., et al., 2006), however, it can have interactions with other medications, so make sure to notify your healthcare practitioner or a pharmacist. It can be taken as a cream or oral medication. Side effects include; headaches, pain, nausea, diarrhea, rashes, liver imbalance – resulting in hepatitis (Martino, M.D., 2011).
Monistat
Treatment using Monistat, a suppository medication (however also available as a cream), can take days and sometimes months to fully eradicate a vaginal yeast infection. It is best to get yourself checked out first before proceeding to the drug store to purchase this medication. There are several side effects to taking Monistat which include; loss of appetite, vomiting, nausea, diarrhea, (you may be allergic to it – skin rashes, hives, itching) feeling cold, fever and pain (Martino, M.D., 2011).
Clotrimazole
This antifungal lotion is usually accompanied by betamethasone (a corticosteroid) and will then go by the common name Lotrisone or Canesten. It is a topical cream, applied to the skin, and should never be placed within the vagina. It does not have any herbal or nutrient interactions, nor have there been any reported nutrient depletions (eds. Gaby, A.R., et al., 2006).
Ketoconazole
This antifungal medication is also from the azole family of antifungals, approved as an oral medication by the FDA in 1981, it is sold as Nizoral. Its use has in many places been replaced by other antifungal medications, however, if it is being prescribed to you and you wish to take medication – ask your doctor/healthcare provider for another alternative. Side effects of ketoconazole include drug interactions, endocrine dysregulation and hepatotoxicity (Gupta, A.K., et al., 2014) Furthermore, as it is absorbed into the bloodstream it has the potential to cause liver damage (Rapp, D., 1991). In a 2016 study on fungal growth in children, coconut oil was shown to be as effective as ketoconazole at the elimination of Candida overgrowth (Shino, B, et al., 2016).

Home Remedies for Vaginal Yeast Infection
Yogurt
Yogurt used internally and externally aids in establishing natural bacterial flora. I have read many accounts of individuals finding this beneficial, my one concern with yogurt is the sugar in it. Many yogurts claim to have health benefits but many of them as simply filled with sugar or artificial sweetener, are pasteurized and though they have healthy bacteria cultures added to them these cultures are usually not alive (healthy bacteria cannot thrive in a pasture environment).
I would personally much rather a garlic clove or coconut oil in my vagina then yogurt. If you so choose to use yogurt make sure that it has very few ingredients, full-fat dairy, and probiotic bacteria, moreover make sure that the yogurt is organic, no sugar added and not pasteurized. Good quality yogurt will be sour when you taste it.
Garlic Clove
I have tried this one myself and recommended it to friends and all of us have found that it works wonders. Granted, if you have allergies to garlic, as with any of these home remedies do not place them in your vagina. I recommend using one organic garlic close, medium in size, peeled. Tie a piece of either string, I like to use natural silk floss because I have it on hand (not mint floss, just plain silk floss). Tie the floss around the garlic clove, if it cuts the clove that’s okay and leaves a fair amount of the floss hanging off so that you can pull it out in the morning. Gently place the garlic clove into your vagina before going to bed (make sure to go pee before putting it in). You may need to repeat this for one to three nights, however, I find that if you catch your yeast infection as soon as it has begun the garlic clove should usually get rid of the candida within one night. It may leave you smelling a little like garlic. Wash yourself off with water as soon as you wake up and by midday, you should be just fine. Garlic has natural antifungal and anti-inflammatory compounds making it a great remedy for kicking Candida out. Always make sure to remove the entire garlic.
In herbal Healing for Women, by Rosemary Gladstar, she suggests wrapping the garlic clove in a thin piece of gauze, a large enough piece so that it leaves a trail at the end making it easy to pull out after use. She recommends changing the garlic suppository every three to five hours. I believe leaving it overnight and during the daytime using other natural remedies will eliminate the yeast just fine.

Coconut Oil for Vaginal Yeast Infection
Caprylic acid is found naturally in coconut oil. This medium-chain fatty acid possesses natural antifungal and anti-yeast properties that can be used to aid in the treatment of a yeast infection. Its short carbon chain allows the caprylic acid to bass the wall of fungus or yeast, destroying the cell membrane and causing the fungus or yeast to separate (Kharrazian, D., 2013). Caprylic acid is one of the most potent antifungals against candida overgrowth. The wonderful thing about coconut oil, as long as you do not have an allergy to it, is that it is safe to be used internally and externally. Consuming it orally daily, aids in diminishing the amount of yeast overgrowth in the digestive system, and applying it internally during a yeast infection, or even using it as a lubricant occasionally can greatly improve the health of the vagina (Fife, B., 2013). Coconut oil is an amazing candida killer. In a 2016 study on fungal growth in children, coconut oil was shown to be as effective as ketoconazole at the elimination of candida overgrowth (Shino, B, et al., 2016).
If you need a lubricant use coconut oil, it works great and unlike petroleum-based products or lubricants that contain harmful chemicals and synthetic perfumes, the use of coconut oil will not result in a yeast infection (Stone, J.J., 2015). When experiencing a vaginal yeast infection, applying coconut oil locally can also aid in soothe and reducing inflammation, which will aid in diminishing the pain and itching associated with the infection (Fife, B., 2013).
Herbal Medicine for Yeast Infections
Herbs that are most beneficial for individuals who are suffering from a vaginal yeast infection are anti-fungal herbs, anti-microbial herbs, immune-stimulating herbs as well as alterative herbs. A combination of herbs from all three of these categorize will be most beneficial in eradicating the effects of candida colonization. When using herbals it is most beneficial to use them in combination, over a long period of time. Combining herbal teas or tincture with a healthy candida eradicating diet as well as other supplements to aid in candida’s elimination will prove to be the most beneficial for suppressing the growth of the yeast throughout the body.
Chamomile
You may be most familiar with chamomiles relaxing qualities, however, it is also anti-inflammatory, antiseptic and a carminative, among other actions. As a carminative, it aids in re-establishing the proper flow and movement of the digestive tract – aiding in the removal of waste products by increasing the release of gastric juices. This may cause some discomfort for a short time. Gastric juices aid in the elimination of bad bacteria and yeast overgrowth (particularly in the small intestine). By reducing the number of bad bacteria and yeast in the digestive tract and increasing good bacteria colonies (through supplementation), the good bacteria will begin to recolonize the vaginal tract as well (Hoffman, D., 1990) (Castleman, M., et al., 1995).
Dosage: 2 tsp in 1 cup of boiling water. Let it steep for between 5-10 minutes.
Berberine
Berberine is not a herb, it is an alkaloid, a plant secondary compound found in barberry, goldenseal and oregano. It has many beneficial actions on the body, such as aiding to heal burnt skin, healing the heart and it possesses anti-bacterial actions. It is very commonly used in Traditional Chinese Medicine as an anti-microbial component one that can be used against candida (Seneviratne, C.J. et al., 2007). This alkaloid has been shown to be effective at the eradication of bacteria, fungus, parasites, worms and viruses in the human body – displaying potent antibiotic actions (Lezak., M., 2000)
Goldenseal can be taken in capsule, as a tincture or tea. It has amazing anti-fungal properties (from the berberine alkaloid within it), as well as being healing to the digestive system. Because digestive health is a mirror image of vaginal health it is important to also address the health and function of the gut as well as the vagina (Stone, J.J., 2015).
Echinacea
This antimicrobial and alterative is one of the best herbal remedies to rid the body of bad microbial overgrowth or infections.
Dosage: 1-2 tsp of dried root steep in boiled water for 5-10 minutes. The coneflower can also be used. I have made it into a tincture by placing a dried coneflower of echinacea into a 40% distillation of alcohol, left to set for about 6 months (shaken every few days or so). However, you can also purchase a tincture at taking 1-2 ml of it 3xdaily or as directed on the bottle (Hoffman, D., 1990).
Marigold
This beautiful flower and herb have amazing actions; it is anti-inflammatory, astringent vulnerary, anti-fungal, a cholagogue, and emmenagogue. It is the anti-fungal action that is the key feature of this herb in its battle against Candida. The other wonderful thing about this herb is that it can be used internally and externally to eradicate fungal infections such as Candida in the vagina (Hoffman, D., 1990).
Dosage: 1-2 tsp steeped in boiled water for 10-15 minutes.
Oil of Oregano
This very strong (somewhat spicy) oil is a powerful anti-fungal herbal medicine. Oil of oregano is also an antiviral and antibacterial as well as aiding in reducing inflammation (Stone, J.J., 2015). In several different studies, oregano has been shown to display profoundly strong actions against bacteria, parasites and fungus (Lezak, M., 2000). However, due to its potency as an antibacterial, it often wipes out both the bad and good bacteria in the digestive system, therefore, it is imperative that you supplement later on in the day with probiotics so that you have them present in your system so that they to can begin repair and continue fighting against the candidal overgrowth.
This oil is to be taken orally in a bit of water or juice when it is in a tincture form. They are also available in capsule form. Both supplements of oil of oregano should be taken on an empty stomach 30 minutes before ingesting food.
Pau d’arco
Pau d’arco is the name of a Brazilian tree (also found natively in Argentina, where it is referred to as Lapacho). The bark of this tree has been used for thousands of years by the natives of Brazil (the Calaway tribe and Incas) to treat and cure diseases and bodily ailments (Tierra, M., 1998)
This wonderful bark has amazing properties and is delicious when enjoyed as a tea. Cooling and slightly bitter, it has wonderful actions that help the body in the eradication of candida such as; alternative, antifungal, antidiabetic, digestive, antibacterial and antitumoral (ibid). It is also a diuretic and can cause the loss of some trace minerals, therefore, it is important to also supplement with a potent multivitamin (Rapp, D., 1991).

References
Antonio, M.A.D., Meyn, L.A., Murray, P.L., Busse, B., Hillier, S.L. (2009). Vaginal Colonization by probiotic Lactobacillus cripatus CTV-05 Is Decreased by Sexual Activity and Endogenous Lactobacilli. The Journal of Infectious Diseases, Volume 199, Issue 10, pages 1506-1513.
Arvigo, R., & Balick, M. J. (1993). Rainforest Remedies: One Hundred Healing Herbs of Belize. Lotus Press: New York.
Batra, S. (2003). The Intimate Self: A Guide To Women’s Sexual Health. Penguin UK: London.
Beigi, R.H., Meyn, L.A., Moore, D.M., Krohn, M.A., Hillier, S.L. (2004). Vaginal Yeast Colonization in Nonpregnant Women: A Longitudinal Study. Obstetrics and Gynecology. Volume 104, Issue 5, page 926-930.
Berkow, E.L., Lockhart, S.R. (2017). Fluconazole resistance in Candida species: A current perspective. Infection and Drug Resistance. Volume 10, pages 237-245.
Brunzel, N.A. (2018). Fundamentals of Urine and Body Fluid Analysis. Elsevier Health Sciences: Missouri.
Castleman, M., Hendler, S.S. (1995). The Healing Herbs: The Ultimate Guide to the Curative Power of Nature’s Medicines. Bantam Books: New York.
CDC. (2017). Vaginal Candidiasis. Center for Disease Control and Prevention. Online Available at CDC.
Chaitow, L. (2016). Candida Albicans: Natural Remedies for Yeast Infection. Simon and Schuster.
Chia, M., & Abrams, R.C. (2006). The Multi-orgasmic Woman: How any woman can Experience Ultimate Pleasure and Dramatically Enhance Her Health and Happiness. Rodale: USA.
Criby, S., Taylor, M., Reid, G. (2009). Vaginal Microbiota and the Use of Probiotics. Interdisciplinary Perspectives on Infectious Diseases.
Fidel. P.L., Vazquez, J.A., & Sobel, J.D. (1999). Candida glabrata: Review of Epidemiology, Pathogenesis and Clinical Disease with Comparison to C.albicans. Clinical Microbiology Reviews. Issue 12, Volume 1, pages 80-96. Online available at PubMed.
Fife, B. (2013). The Coconut Oil Miracle, 5th Edition. Penguin Books: New York.
Greene, C.D. (2012). Permanently beat Yeast Infection & Candida: proven Step-by-Step Cure for Yeast Infections and Candidiasis, Natural, lasting Treatment That Will prevent Recurring Infection. Woman’s Republic: Georgia.
Gupta, A.K., Daigle, D., Foley, K.A. (2014). Drug Safety Assessment of Oral Formulations of Ketoconazole. Expert Opinion on Drug Safety. Volume 14, Issue 2, pages 325-334.
Hoffman, D. (1999). Holistic Herbal. A Safe and Practical Guide to Making and Using Herbal Remedies. Thorsons: London.
Jespers, V., van de Wijgert, J., Cools, P., Verhelst, R., Verstraelen, H., Delany-Moretlwe, S., … for the Vaginal Biomarkers Study Group. (2015). The significance of Lactobacillus crispatus and L. vaginalis for vaginal health and the negative effect of recent sex: a cross-sectional descriptive study across groups of African women. BMC Infectious Diseases, 15, 115. Online Available at PubMed.
Jin, L., Tao, L., Pavlova, S.I., So, J.S., Kiwanuka, N., Namukwaya, Z., Saberbein, B.A., Wawer, M. (2007). Species diversity and relative abundance of vaginal lactic acid bacteria from women in Uganda and Korea. Journal of Applied Microbiology. Volume 102, issue 4, pages 1107-1115. Online Available at PubMed.
Junger, A. (2013). Clean Gut. Harper One: New York.
Lezak., M. (2000). Herbal Antimicrobials for Intestinal Infections. Advanced Nutriton Publications.
Linhares, I.M., Summers, P.R., Larsen, B., Giraldo, P.C., Witkin, S.S. (2011). Contemporary perspectives on vaginal pH and lactobacilli. American Journal of Obstetrics and Gynecology. Volume 204, Issue 2, pages 120.e1-120.e5. Online Available at PubMed.
Martino, M.D. (2011). Natural Health: Alternatives and Prevention of Disease. Author House: Indiana.
Mindell, E. (2004). Probiotics. Basic Health Publications: New York.
Murkoff, H., Eisenbeg, A., Hathaway, S. (2002). What to Expect When You’re Expecting. Workman, Publishing: New York.
Nobile, C.J., & Johnson, A.D. (2015). Candida albicans Biofilms and Human Disease. Annual Review of Microbiology. Volume 69, pages 71-92. Online Available at PubMed.
Pfaller, M. A., Diekema, D. J., Gibbs, D. L., Newell, V. A., Nagy, E., Dobiasova, S., … the Global Antifungal Surveillance Group. (2008). Candida krusei, a Multidrug-Resistant Opportunistic Fungal Pathogen: Geographic and Temporal Trends from the ARTEMIS DISK Antifungal Surveillance Program, 2001 to 2005. Journal of Clinical Microbiology, 46(2), 515–521. Online Available at PubMed.
ed. Prasad, R. (2017). Candida albicans: Cellular and Molecular Biology. Springer: Inda.
Rapp, D. (1991). Is this Your Child? Discovering and Treating Unrecognized Allergies in Children and Adults. William Morrow: New York.
Ross, J. (2012). The Diet Cure: The 8-Step program to Rebalance your Body Chemistry and End Food Cravings, Weight Gain and Mood Swings Naturally. Penguin: New York.
Sanguinetti, M., Posteraro, B., Lass, F.K. (2015). Antifungal Drug resistance Among Candida Species: Mechanisms and Clinical Impact. Mycoses. Volume 58, Issue 2, Pages 2-13.
Ed. Schlossberg, D. (2008). Clinical Infectious Disease. Cambridge University Press: Cambridge.
Seneviratne, C.J., Wong, R.W.K., Samaranayake, L.S. (2007). Potential anti-microbial activity of traditional Chinese medicine herbs against Candida species. Mycoses. Volume 51, Issue 1, page 30-34. Online Available at PubMed.
Shina, B., Peedikayil, F.C., Jaiprakash, S.R., Bijapur, G.A., Kottayi, S., Jose, D. (2016). Comparision of Antimicrobial Activity of Chlorhexidine, Coconut Oil, probiotics and ketoconazole on Candida albicans isolated in Children with Early Childhood Caries: An In Vitro Study. Scientifica, Article ID 7061587.
Stephen E. Hawes, Sharon L. Hillier, Jacqueline Benedetti, Claire E. Stevens, Laura A. Koutsky, Pål Wølner-Hanssen, King K. Holmes; Hydrogen Peroxide—Producing Lactobacilli and Acquisition of Vaginal Infections, The Journal of Infectious Diseases, Volume 174, Issue 5, 1 November 1996, Pages 1058–1063. Online available at PubMed.
Stone, J.J. (2015). No More Yeast Infection: The Complete Guide on Yeast Infection Symptoms, Causes, Treatments and A Holistic Approach to Cure Yeast Infection. Eliminate Candida, Naturally & Permanently. Living Plus Healthy Publishing: United States.
eds. Sweet, R.L., & Gibbs, R.S. (2009). Infectious Diseases of the Female Genital Tract. Wooltersklumer; New York.
Tierra, M. (1998). The Way of Herbs. Pocket Books: New York.
Trofa, D., Gácser, A., & Nosanchuk, J. D. (2008). Candida parapsilosis, an Emerging Fungal Pathogen. Clinical Microbiology Reviews, 21(4), 606–625. Online Available on PubMed.
Whaley, S.G., Berkow, E.L., Rybak, J.M., Nishimoto, A.T., Barker, K.S., Rogers, P.D., (2016). Azole Anti Fungal Resistance in Candida albicans and Emerging Non-albicans Candida. Frontiers in Microbiology. 7, 2173.
Zuza-Alves, D.L., Silva-Rocha, W.P., Chaves, G.K. (2017). An Update on Candida tropicalis Based on Basic and Clinical Approaches. Frontiers in Microbiology.
Amanda Filipowicz is a certified nutritional practitioner (CNP) with a bachelor in environmental studies (BES) from York University. She also has certification in clinical detoxification, prenatal and postnatal care as well as nutrition for mental health. She has been working as a nutritionist since 2013 and is a lifelong proponent of eating healthy.

