Do you ever get heartburn? The surprising thing, heartburn is a symptom that you are lacking in stomach acid. You most likely have low stomach acid and are experiencing acid reflux. There are no symptoms of heartburn because heartburn itself is a symptom of acid reflux (Lipski, E., 2015).
Acid reflux is also known as gastroesophageal reflux disease or GERD and one of the main symptoms is heartburn. GERD is chronic acid reflux or relapsing acid-peptide disorder which results in gastric juices refluxing into the esophagus (which we experience as heartburn). Heartburn is only a symptom, but it is when acid reflux gets to the point of damaging esophageal tissues and displaying a negative result on human health that it is diagnosed as gastroesophageal reflux disorder (GERD) (eds. Buchler, M., et al., 1997) (Enders, G., 2015).
If left untreated it can lead to the development of cancer of the esophagus. Acid reflux begins to be a problem when it is experienced more than twice a week, what this means is that if you are experiencing heartburn more than twice a week you may need to consider addressing the issue. If you want to know how to get rid of heartburn, you need to know why acid reflux happens in the first place. This way you can prevent GERD from occurring (eds. Sharma, P., et al., 2018).
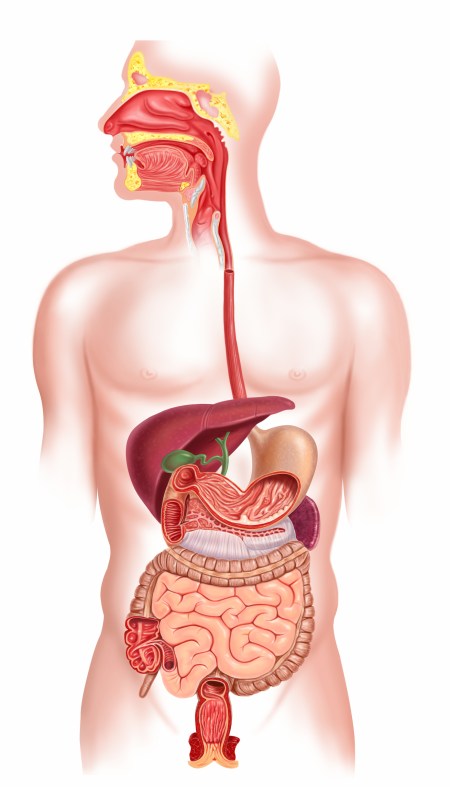
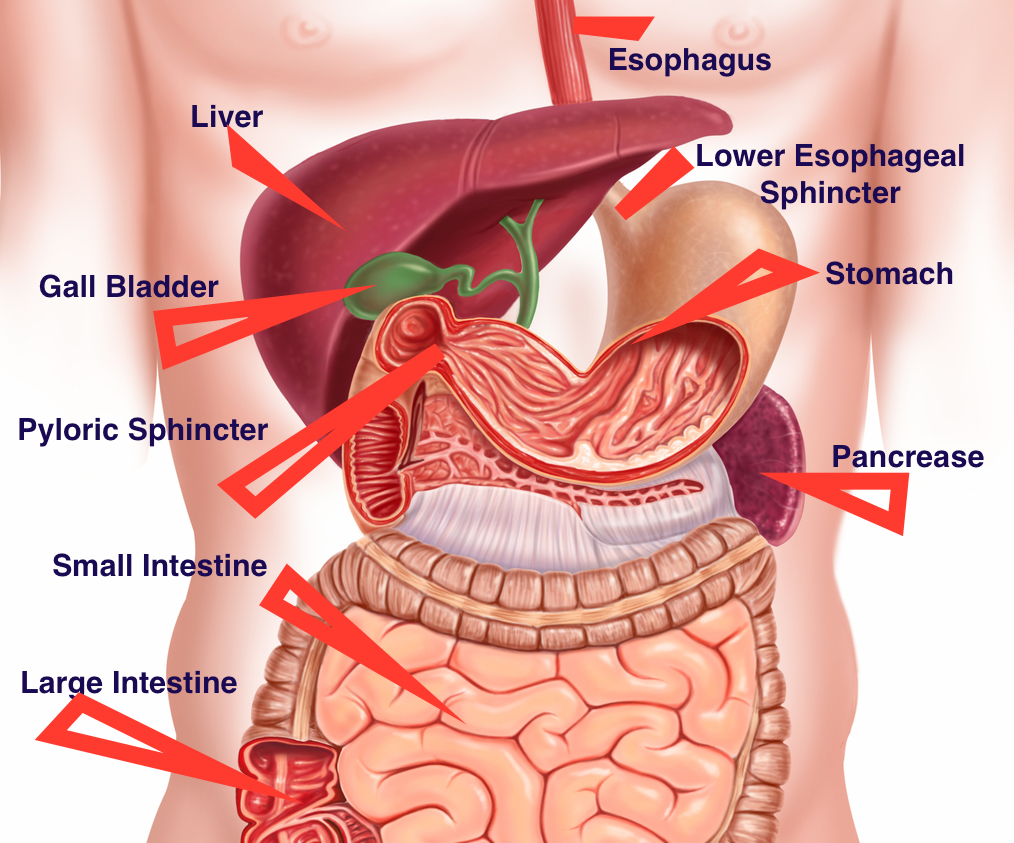
First, we begin with the configuration of the esophagus and the stomach. The esophagus and the stomach are joined together by the lower esophageal sphincter (LES), this sphincter should only open under two circumstances; 1) Food/drink is entering into the stomach (the chewing and swallowing of nutrients), 2) the release of gas from the stomach (Enders, G., 2015) (Lipski, E., 2015).
The main role of acid in the stomach is to break down food. With too little acid, food cannot be properly broken down and therefore it ferments. Fermentation brings about intra-abdominal pressure (IAP), resulting in gas and that leads to the opening of the LES – thus welcoming acid reflux and the symptom of heartburn. Unlike the stomach, which is coated in mucus, the esophagus does not have a protective coating for its cell lining (Lipski, E., 2015).
IAP can also be agitated by the consumption of the Standard American Diet. Included are processed foods, foods high in fructose (when things get really bad even fruits – especially for individuals who are intolerant/have trouble breaking down fructose) and carbohydrates. These foods ferment very quickly, feeding bad bacteria in the stomach and, with low acid in the stomach they more easily produce gas, hence stimulating the LES to open and acid to splash into the esophagus (eds. Sharma, P., et al., 2018).
A good place to start to heal is to reduce the consumption of foods/drinks that relax the LES. This includes…
- alcohol
- coffee – even decaf
- chocolate
- spicy foods
- fatty foods; deep-fried, margarine
- peppermint
- citrus fruits
- tomatoes (nightshades in general)
- calcium supplements
You don’t need to take them all out at once. Work through the list mindfully and see what you can replace so that your life can go on pleasantly. Coffee, for example (this goes for decaf as well) can be replaced with dandelion root coffee or an adrenal formula (Strest by St. Francis is an adaptogen you will need to use it consecutively to see results – make sure to speak with your doctor before taking it if you are on medication incase there as interactions to the herbs).
Another great thing to do is to take deep breaths, meditate or give thanks before a meal. Ground your body and let it relax so that you can switch from “fight or flight” mode into “rest and digest”. So next time you sit down for a meal check-in with yourself, see how you are doing, are you offbeat or restless? If so take a moment and bring yourself back to earth.
Why do we get low stomach acid?
- chronic stress – stress is a mind killer, affecting nerves in the body and placing the body off balance.
- age – stomach acid production is reduced with age.
- H.Pylori bacteria – destroys parietal cells of the stomach lining.
- PPI – Proton Pump Inhibitor – reduces stomach acid to almost nothing.
Why is stomach acid important?
- begins the breakdown of fat and protein
- digests food and breaks it down so that when it moves into the small intestine it will stimulate the gallbladder to release bile and the pancreas to release pancreatic enzymes.
- when the body’s pH is too high (a signal of low stomach acid) minerals and vitamins can not/have a hard being absorbed by the body
- Vitamins bound to protein (such as B vitamins) cannot be unbound without being properly broken down by stomach acid.
- without the right amount of stomach acid, malabsorption of food occurs possibly leading to malnutrition (Gottschall, E.G., 1994).
How does this relate to bloating?
Digestion begins in the mouth. Certain foods, especially foods with starch, need to be properly broken down in the mouth to effectively digest in the stomach and gut. For instance; if starch is not broken down in the mouth (into dextrin) the next step in the gut cannot continue (dextrin moves through the stomach to the gut where it is broken down into maltose).
Stomach acid is needed to break down your food further. Chewing food properly is a great way to kick-start good digestion but the stomach is where protein and fats begin to break down. If the digesting food hangs out in the stomach for too long, fermenting and mixing up without reaching the proper pH level ( between 1-3, closer to 2) the entire process is thrown off.
The pyloric sphincter (the connecting passageway between the stomach and the small intestine) will slowly let digested food into the small intestine (where it will become chyme). If our food has not reached the proper pH yet has entered the small intestine it may or may not stimulate the pancreas to release pancreatic enzymes and digestive juices and the gallbladder to release bile needed to both neutralize the chyme and continue the digestive process (Cutler, E.W., et al., 2005) (Ghoshal, U., et al., 2014) (Hod, K., et al., 2014).
This is by no means comfortable for the intestines and in all likelihood they may become slightly inflamed – attributing to bloating.
Other reasons we might be experiencing Heartburn…
- A hiatus hernia
- Pregnancy
- Lower Abdominal Fat
References
Eds. Buchler, M., Frei, E., Klaiber, Ch., Krahenbuhl, L. (1997). Gastroesophageal Reflux Disorder (GERD), Back to Surgery. Karger: London.
Cutler, E. W., & Kaslow, J. E. (2005). Micromiracles: Discover the healing power of enzymes. United States: St. Martin’s Press.
Enders, G. (2015). Gut: The inside story of our body’s most under-rated organ. Australia: Scribe Publications.
Ghoshal, U., Shukla, R., Ghoshal.U.C., & Dhole, T. N. (2014). Fecal Microbiota in patients with irritable bowel syndrome compared to healthy controls by real-time PCR: An evidence of Dysbiosis. Gastroenterology, 146(5)
Gottfried, S., & Northrup, C. (2013). The hormone cure: Reclaim balance, sleep, sex drive, and vitality naturally with the Gottfried protocol. Philadelphia, PA, United States: Scribner.
Gottschall, E. G. (1994). Breaking the vicious cycle: Intestinal health through diet. Baltimore, Ontario: The Kirkton Press.
Hod, K., Ringel-Kulka, T., Van Tilburg, M. A., & Ringel, Y. (2014). Abdominal bloating in patients with irritable bowel syndrome: Characterization of clinical symptoms, psychological factors and associated Comorbidities. Gastroenterology, 146(5), S–532.
Lipski, E. (2011). Digestive Wellness: Strengthen the immune system and prevent disease through healthy digestion, fourth edition (4th ed.). New York, NY: McGraw-Hill Professional Publishing.
eds. Sharma, P., Bhatia, S., Goh, K.L. (2018). The Rise of Acid Reflux in Asia. Springer: New Delhi.
Amanda Filipowicz is a certified nutritional practitioner (CNP) with a bachelor in environmental studies (BES) from York University. She also has certification in clinical detoxification, prenatal and postnatal care as well as nutrition for mental health. She has been working as a nutritionist since 2013 and is a lifelong proponent of eating healthy.